- 2 weeks ago
- 20Minutes
- 5026Words
- 2490Views
Crohn’s Disease Treatment. There is hope!
Being one of the most painful and difficult digestive complaints to treat, Crohn’s disease is a growing problem worldwide. It can be confused with Ulcerative colitis, irritable bowel syndrome, and gastric ulcers. If you are suffering from it you may find yourself quite despairing when looking for treatment solutions. This is because the cause and cure alike are almost a complete mystery to modern medicine. Crohn’s disease treatment is seen as an attempt to reduce symptoms, while a Crohn’s disease cure has still not been discovered. The time has now come to open up your options.
(1) In vitro activity of Aloe vera inner gel against Helicobacter pylori strains. PUBMED https://www.ncbi.nlm.nih.gov/pubmed/24597562
(2) Recurrent aphthous stomatitis and Helicobacter pylori. PUBMED https://www.ncbi.nlm.nih.gov/pubmed/26827061
(3) The relationship of recurrent aphthous stomatitis and Helicobacter pylori, cytokine gene polymorphism and cobalamin. PUBMED https://www.ncbi.nlm.nih.gov/pubmed/26039006
(4) Slippery Elm Overview, University of Maryland. http://umm.edu/health/medical/altmed/herb/slippery-elm
(5) Bitters: Time for a New Paradigm. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4446506/
(6) Crohn’s disease: a clinical update. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4622286/
(7) Inflammation, Antibiotics, and Diet as Environmental Stressors of the Gut Microbiome in Pediatric Crohn’s Disease. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4633303/
(8) High School Diet and Risk of Crohn’s Disease and Ulcerative Colitis. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4567521/
(9) Diet therapy for inflammatory bowel diseases: The established and the new. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4734995/
(10) Herbal and plant therapy in patients with inflammatory bowel disease. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4367210/
(11) Effect of licorice versus bismuth on eradication of Helicobacter pylori in patients with peptic ulcer disease. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4166824/
(12) ALTERNATIVE MEDICINE PRODUCTS AS A NOVEL TREATMENT STRATEGY FOR INFLAMMATORY BOWEL DISEASE. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2596578/
(13) Genes, emotions and gut microbiota: The next frontier for the gastroenterologist. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5423040/
(14) Berberine promotes recovery of colitis and inhibits inflammatory responses in colonic macrophages and epithelial cells in DSS-treated mice. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3311435/
(15) Steroid-sparing effect of wormwood (Artemisia absinthium) in Crohn’s disease: a double-blind placebo-controlled study. PUBMED https://www.ncbi.nlm.nih.gov/pubmed/17240130/
(16) Randomized, double-blind, placebo-controlled trial of oral aloe vera gel for active ulcerative colitis. PUBMED https://www.ncbi.nlm.nih.gov/pubmed/15043514
(17) Antiulcerogenic effects of coconut (Cocos nucifera) extract in rats. PUBMED https://www.ncbi.nlm.nih.gov/pubmed/18521965
(18) Manuka Honey Exerts Antioxidant and Anti-Inflammatory Activities That Promote Healing of Acetic Acid-Induced Gastric Ulcer in Rats. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5307292/
(19) Effectiveness of Citrus Fruits on Helicobacter pylori. PUBMED https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5376954/
Today I will share with you the holistic view, covering food, herbs, and mind-body medicine giving you a new ray of hope. Many people have completed our program and reported success at relieving the symptoms of Crohn’s disease. The key to healing is to make the complex simple, and this is what I will aim to achieve. Simple natural solutions may require a little effort but can be well worth the reward. Life’s journey is all about learning, growing, and ultimately healing, Let’s begin.
What is Crohn's Disease
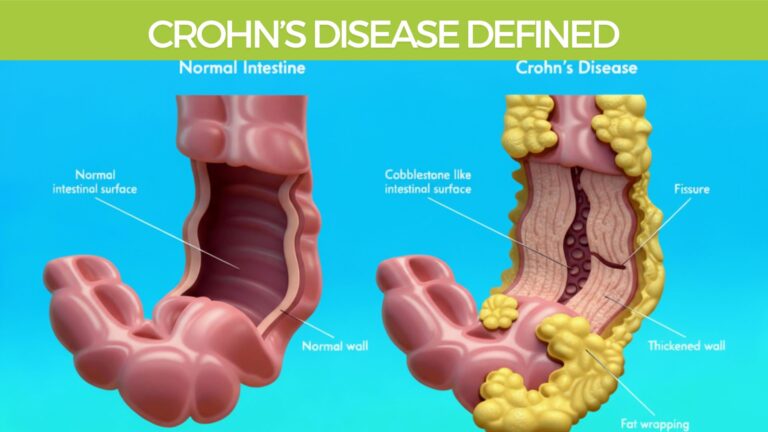
Crohn’s disease (CD) is a chronic, relapsing inflammatory bowel disease (IBD).
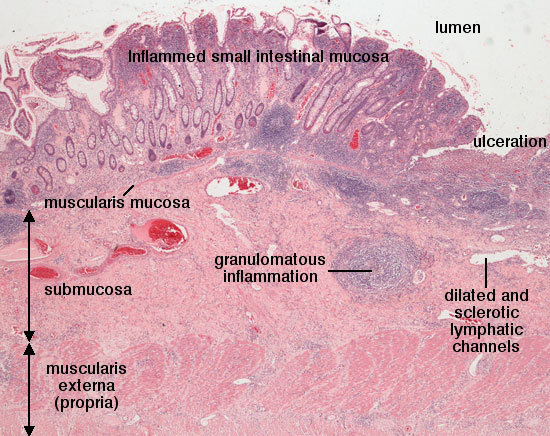
It is characterized by transmural granulomatous inflammation (deep ulcers) that can affect any part of the gastrointestinal (GI) tract.
Most commonly affected areas:
- Ileum (last section of the small intestine).
- Colon (large intestine).
- Often involves both the small and large intestines.
Prevalence:
- Affects approximately 1 in 500–700 people.
- Prevalence has continually increased over the past 50 years.
- Highest incidence reported in Northern Europe, the United Kingdom, and North America.
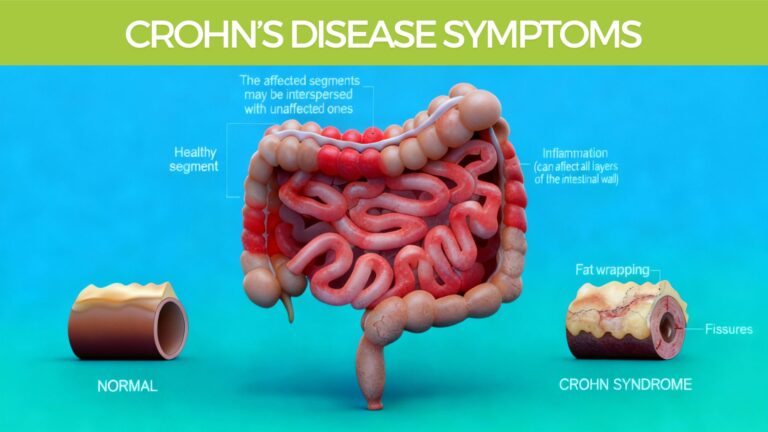
Location in the GI tract:
While Crohn’s most commonly affects the intestines, it may occur anywhere from the mouth to the anus.
Early stages:
- The condition begins with small ulcers in the gut lining, known as aphthous ulcers.
- These are similar in appearance to mouth ulcers.
Who is most affected:
- More common between the ages of 15–40 years.
- Higher risk in smokers.
- Can run in families, suggesting genetic susceptibility.
Gender differences by region:
- In Canada and New Zealand, females are 10–30% more likely to develop Crohn’s than males.
- In Japan and Korea, males are reported to be up to three times more likely to develop Crohn’s than females. (6)
Crohn's Disease Symptoms
Crohn’s disease symptoms vary in intensity over time and depend on what part of the Gastrointestinal tract is affected. Because the disease stems from inflammation deep in the intestinal wall called granulomatous inflammation (see diagram) and often results in ulceration. Crohn’s disease symptoms can be wide-reaching.
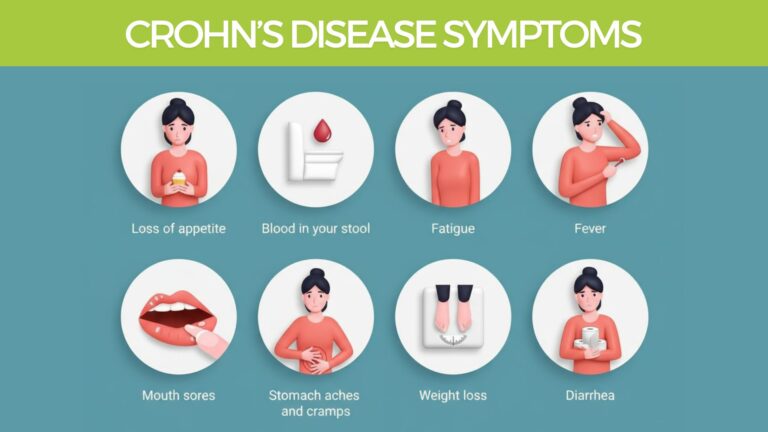
Most common symptoms:
- Abdominal cramps and pain
- Loss of appetite
- Unintentional weight loss
- Pain when passing stool
- Persistent, watery diarrhea (lasting more than 4 weeks)
- Blood and mucus in stools
- Swollen gums
- Increased human DNA detected in feces (indicator of gut lining damage)
Less common symptoms (affecting ~35% of patients):
- Mouth ulcers (similar to aphthous ulcers)
- Peripheral joint pain and swelling (arthritis-like symptoms)
- Erythema nodosum – fatty inflammation beneath the skin causing tender red nodules
- Ankylosing spondylitis – inflammatory arthritis of the spine and sacroiliac joints
- Eye inflammation (such as uveitis or episcleritis)
Very rare symptoms:
- Psoriasis – autoimmune skin condition causing scaly patches
- Pyoderma gangrenosum – painful necrotic ulcers on the legs
- Primary sclerosing cholangitis (PSC) – chronic inflammation of the bile ducts
Crohn's Disease Diagnosis
No single definitive test exists for diagnosing Crohn’s disease (CD).
The most widely used diagnostic method is full ileocolonoscopy with biopsies. (6)
Imaging and visual investigations:
- Ultrasound, CT scan, and MRI can all detect Crohn’s-related changes.
- A cross-sectional analysis using all three methods provides up to 90% accuracy in diagnosis.
Capsule endoscopy:
- A relatively new, non-invasive imaging technique.
- Involves swallowing a small, disposable capsule with a wireless camera.
- Allows direct visualization of the small bowel mucosa as it passes through the GI tract.
Evidence from meta-analysis:
- Capsule endoscopy has shown an increased diagnostic yield of 15% compared to other imaging methods. (6)
- Laboratory antibody testing:
- Certain antibodies are associated with Crohn’s disease:
- Perinuclear anti-neutrophil cytoplasmic antibodies (pANCA).
- Anti-Saccharomyces cerevisiae antibodies (ASCA).
Identifying these markers can help differentiate Crohn’s disease from ulcerative colitis when diagnosis is uncertain. (6)
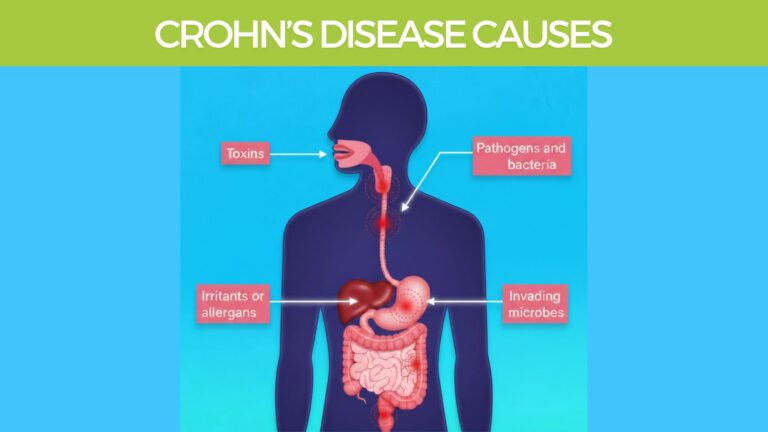
What causes Crohn’s disease?
This is where things can get a little more rocky and difficult to pin down, as the causes can be multi-faceted and complex.
However with a little digging and through a process of elimination you can get the root causes and deal with them appropriately.
Allopathic medicine perspective:
The exact cause of Crohn’s disease (CD) remains a mystery. This is often the case with mainstream medical diagnosis, espeically when the cause is multi-facted and potentially environmental, stress, and toxin related.
It is classified as an autoimmune disorder:
The immune system mistakenly attacks and damages healthy body tissue.
In Crohn’s, the immune system targets the intestinal lining.
Why does the body attack itself?
Likely because gut tissue appears foreign due to irritants or invaders.
Common triggers of an immune response include:
- Toxins (Environmental or Ingested)
- Irritants or allergens
- Pathogens and bacteria
- Other invading microbes
Helicobacter pylori link:
The bacterium Helicobacter pylori has been detected in the oral mucosa or ulcerated lesions of some patients with recurrent aphthous ulcers, which resemble those found in Crohn’s disease. (2)
Antibody and microbiome connection:
In Crohn’s patients, the immune system produces the following:
- pANCA antibodies
- ASCA antibodies
These likely result from an abnormal immune response to intestinal flora (gut microbiota).
Suggests a direct link between gut bacteria balance and Crohn’s disease.
How gut imbalance drives autoimmune attack:
When the gut microbiota is out of balance and overpopulated with harmful bacteria like H. pylori:
- The immune system is activated to attack the invader.
- Over time, the immune system becomes confused and begins to attack the intestinal lining itself.
- This triggers a cascade of inflammation leading to chronic autoimmune activity.
Holistic common-sense approach:
- Support a healthy gut microbiome.
- Reduce inflammation naturally.
- Encourage intestinal wall healing.
- Promote balanced immune responses.
- Use natural methods to help knock back H. pylori.
These goals can be achieved with a holistic approach using natural foods and medicinal herbs
Crohn's Disease Conventional Treatment
While the mainstream medical establishment are still saying the cause of Crohn’s disease is unkown, the standard approach used to treat most auto-immune related inflammatory diseases is used, and is outlined below.
Corticosteroids:
Commonly prescribed for inducing remission in Crohn’s disease.
Not suitable for long-term maintenance because of:
- Increasing resistance over time.
- Risk of patient dependence.
- Significant adverse side effects with prolonged use.
Anti-inflammatory drugs:
- 5-aminosalicylates (5-ASA) have a long history of use.
- Shown to be ineffective in bringing lasting remission or preventing relapse. (6)
Immunosuppressant drugs:
- Another primary pharmaceutical option.
- Aim to suppress immune activity but do not resolve the root cause of Crohn’s disease.
Limitations of pharmaceuticals:
Current drug-based treatments do not:
- Address the underlying causes of Crohn’s disease.
- Promote true intestinal healing.
- In severe or unresponsive cases, surgery often becomes the last resort.
Turning to natural solutions:
Unlike drugs, foods and herbs can support healing at the root level.
Natural approaches aim to:
- Reduce inflammation naturally.
- Repair the intestinal lining.
- Support a healthy gut microbiome.
- Eliminate and reduce exposure to potential toxins
- Address the Body-Mind connection
This is where nutritional therapy and herbal medicine step in.
First step: start with healing foods.
Aggravating Factors
Just a quick refresher and what can be the underlying cause of sypmtoms we aim to address naturally.
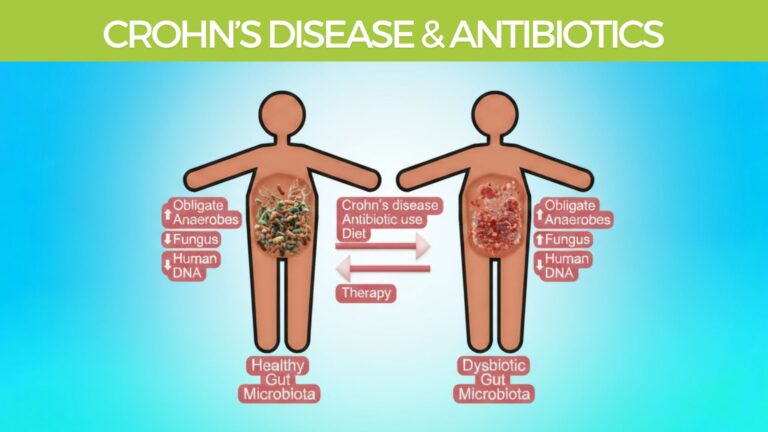
Gut microbiota disturbances are strongly associated with:
- Intestinal inflammation.
- Antibiotic use, which increases gut dysbiosis (imbalance of gut bacteria).
- Reduced inflammation correlates with improved microbial balance.
Fungal overgrowth in Crohn’s disease:
- Candida species, especially Candida albicans, are often elevated in Crohn’s patients.
- Fungal proportions rise with both disease activity and antibiotic use.

Crohn's Disease Diet Principles
Let’s look into the practical ways diet can be used to reduce the underlying causes and potentiallyh reduce the syptomsd of Crohn’s Disease.
Dietary therapy and microbiota:
Diet can rapidly change gut microbiota composition, in ways distinct from other stress-related changes.
Effective dietary interventions can reduce inflammation naturally.
Findings suggest that dysbiosis in Crohn’s results from a combination of:
- Inflammation.
- Dietary patterns.
- Antibiotic exposure. (7)
Dietary risk and protection factors
Increased Crohn’s disease risk has been linked to:
- High intake of fats, especially polyunsaturated omega-6 fatty acids.
- Red meat and processed meats.
- Trans-fats (processed fats) which are highly inflammatory.
Protective dietary factors:
- High intake of dietary fiber.
- Fruits and vegetables. (6)
Knowledge gaps:
Limited research on how gut microbes respond to environmental stressors.
Still unclear whether dysbiosis caused by inflammation can be quickly reversed.
Patients with Crohn’s are often exposed to antibiotics and dietary changes, both of which can alter microbiota balance in unpredictable ways.
Dysbiotic Crohn’s disease has been linked with:
- Increased Candida overgrowth.
- Prior antibiotic therapy.
- Higher concentrations of human DNA in feces, indicating tissue damage. (7)
Natural treatment insights:
A combination of:
- Probiotics, especially obligate anaerobes (beneficial bacteria for colon health).
- An anti-inflammatory, antifungal diet.
- Supportive herbs with antimicrobial and gut-healing properties.
Together, these may promote long-term healing and microbiome balance in Crohn’s disease.
Practical takeaway for diet:
A good Crohn’s disease diet plan should include:
- Plenty of fruits, vegetables, and herbs.
- Foods rich in healthy microorganisms to repopulate the gut.
A focus on natural, plant-based, anti-inflammatory nutrition.
Crohn's Disease Diet Plan In-Depth
To address the underlying causes and aggravating factors of Crohn’s disease altering the diet is crucial.
Below I will outline the foods to avoid, and foods to eat more of, and suggest some herbs and spices that can be added to your recipes.

Foods to Avoid in Crohn’s Disease
Gas- and diarrhea-triggering vegetables:
- Brassicas such as cauliflower, Brussels sprouts, cabbage, asparagus, and broccoli.
- Excess beans and chickpeas can also worsen bloating and diarrhea.
Excessively high-fiber or roughage foods:
- Bran, beans, nuts, and seeds can irritate the gut lining and worsen symptoms.
Fatty, greasy, or fried foods:
- Overcooked, deep-fried, and greasy foods are difficult to digest and can aggravate inflammation.
Processed and packaged foods:
- Items such as cereals, crackers, crisps, nachos, tacos, biscuits, and snack foods.
- These often contain preservatives, artificial additives, or unhealthy fats.
Nightshade family foods:
- Includes potatoes, tomatoes, capsicums (bell peppers).
Especially important: avoid smoking tobacco, which worsens inflammation and Crohn’s progression.
Gluten-containing foods:
- Such as bread, pasta, pastries, cakes, muffins, buns, bagels, and slices.
- Gluten may worsen inflammation and digestive symptoms in Crohn’s patients.
Spices and exceptions:
- Many hot spices can irritate the gut, However, cayenne pepper is an exception:
- Shown to help reduce ulcers, pain, and inflammation.
- May inhibit the growth of Helicobacter pylori, a bacterium linked to Crohn’s disease.
Medical nutrition therapy (tube feeding):
- Studies support tube feeding as effective as corticosteroids in inducing remission.
- Also shows better outcomes for growth and mucosal healing.
- However, it may only be practical in hospital settings, limiting quality of life.
General principle for Crohn’s healing:
- The easier food is to digest, the more the gut can rest and heal.
- Smaller meals of easily digestible fruits and vegetables.
- Increased liquid intake supports healing and hydration. (9)

Foods to eat more of on the Crohn's diet:
Coconut milk & oil
A rat study showed both coconut milk and coconut water protect the ulcerated gut wall.
Coconut milk reduced ulcer size by 54%, while coconut water reduced it by 39%.
Recommendation: Use coconut milk regularly and cook with coconut oil. (17)
Manuka honey
Animal research found Manuka honey effective for:
Healing chronic ulcers.
Preserving mucosal glycoproteins (protective gut lining compounds).
Benefits come from its antioxidant and anti-inflammatory properties. (18)
Citrus fruits
Compounds from citrus fruits have been studied for:
Reducing Helicobacter pylori activity.
Lowering risk of gastric carcinoma.
Inhibiting urease enzyme activity (linked to ulcer formation).
Suggests citrus, alone or with antibiotics, may help eradicate H. pylori and prevent ulcer relapse. (19)
Soothing and gut-healing foods
Eat foods that are easy to digest and calming to the gut:
Stewed apples with cinnamon
Avocado
Salmon
Brown rice
Porridge (oats)
Vegetable soups and broths
Plain, unsweetened yogurt
Probiotic and prebiotic foods
Support a healthy gut microbiome with:
Kefir
Plain yogurt
Sauerkraut
Fiber from fresh vegetables and fish intake have both been shown to reduce Crohn’s disease risk. (8)
Eating style tips
Eat smaller, frequent meals instead of large meals.
Drink plenty of water throughout the day to support digestion and healing.
Culinary and digestive herbs for Crohn’s diet
Regularly include anti-inflammatory and digestive herbs:
Basil, Cayenne, Cinnamon, Cloves, Mixed herbs, Nutmeg, Oregano, Parsley, Rosemary, Thyme, Turmeric.
Benefits:
Reduce inflammation.
Support digestion.
Balance gut microbiota.
Practical tip: Add these herbs into vegetable soups, mild curries, or stir-fries.
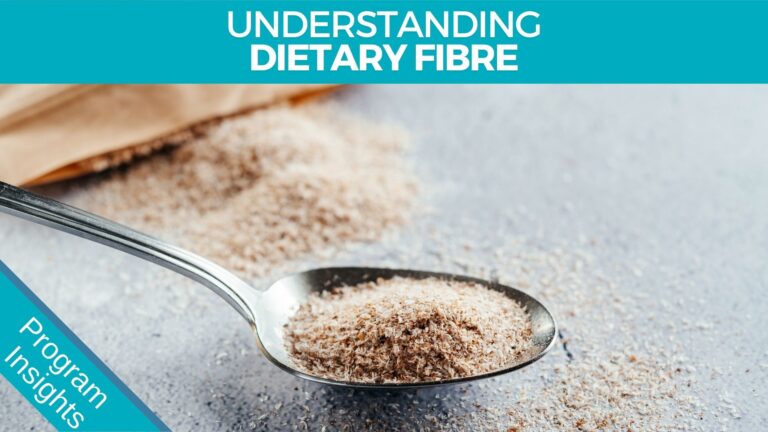
Dietary Fibre & Gut Health
Diet directly impacts gut microbiota diversity because resident micro-organisms obtain energy for growth through the metabolism of dietary nutrients. (13)
Therefore, food choices shape the balance of beneficial vs. harmful gut bacteria.
Global population studies report consistent findings:
- Low-fat, high-fiber diets → associated with greater populations of beneficial bacteria.
- High-fat diets → associated with increases in harmful, pro-inflammatory bacteria.
- Long-term stool sample analysis confirmed the protective role of dietary fiber in supporting a healthy gut microbiome.
Impact of Westernized diets:
Even short-term dietary changes to a Western-style diet (high animal fat, high sugar, low fiber) can:
- Rapidly alter the composition and metabolism of gut flora.
- Decrease beneficial bacteria levels.
- Increase bile-tolerant, inflammation-associated bacteria. (13)
Practical takeaway:
Diets rich in plant-based fiber (fruits, vegetables, legumes, whole foods) support a healthy gut microbiome.
Limiting high-fat, high-sugar, and processed foods helps reduce Crohn’s-related gut dysbiosis
Medicinal Herbs for Crohn's Disease
General findings:
- Many studies show favorable results from herbal and plant-based therapies in inflammatory bowel disease (IBD). (12)
- Herbal remedies may reduce inflammation, support gut healing, and aid in long-term remission.
Aloe Vera
Benefits:
- Helps heal ulcers and reduces pain.
- Inner gel shows antibacterial activity against both resistant and non-resistant Helicobacter pylori strains. (1)
- Especially useful for patients with aphthous ulcers linked to H. pylori. (3)
Clinical trial:
- In a double-blind, placebo-controlled study (44 patients, mild–moderate ulcerative colitis):
- Oral aloe vera gel (100 mL daily for 4 weeks) led to more frequent clinical response, reduced histological activity, and was safe. (10, 16)
Slippery Elm Bark
Benefits:
- Contains mucilage, which becomes a soothing gel coating the GI tract.
- Relieves pain and protects against ulcers and excess acidity.
- Stimulates mucus secretion, providing a natural protective barrier. (4)
Licorice Root
Benefits:
- Shows anti-ulcer activity comparable to common ulcer medications. (12)
- Clinical evidence suggests licorice is as effective as bismuth in eradicating H. pylori. (11)

Golden Seal
Key compound: Berberine.
Benefits:
- Used for bacterial diarrhea and intestinal parasite infections.
- Recent studies show berberine also has anti-inflammatory effects. (14)

Wormwood
Clinical study:
- 18 Crohn’s patients given wormwood showed steady improvement, even while tapering steroids.
- After 8 weeks:
65% achieved near-complete remission.
None in the placebo group achieved remission.
- Benefits persisted through week 20 without steroid reintroduction. (15)
Herbal Bitters (liquid blend, 2.5 mL before meals)
Herbal Bitters are traditionally used as tonics for the entire digestive function, as bitter compounds known as bitter principles stimulate the digestive organs via the vagus nerve.
Common herbs: Goldenseal, Wormwood, Gentian, Andrographis, Milk Thistle, Dandelion, Globe Artichoke, Gymnema.
Benefits:
- Stimulate gustatory nerves, increasing secretion of gastric juices and bile.
- Promote appetite, digestion, and liver support.
- Help reduce negative bacteria and gut inflammation. (5)

Herbal Teas
Herbal teas also have a long history of improving digestion and soothing inflammation of the gut.
Soothing teas include: Chamomile, Peppermint, Ginger, and Fennel.
Benefits:
Reduce pain and inflammation.
Encourage digestive healing.
Holistic herbal approach
Using a combination of these herbs maximizes results.
Natural treatments usually bring gradual healing over months.
Long-term results are possible with consistency and patience.
Many of these remedies are combined in the Ultimate Crohn’s Disease Program (see below).
Body-Mind Crohn’s Disease Medicine
It’s always important to incorporate some kind of body mind approach to any disease or disorder, as similar to the placebo effect has shown the mind has incredible power over the body.
This means that whatever you think will manifest itself in someway in the body and utilising the power of the mind to heal can be profound.
Let’s look at this briefly.
The Gut Brain Connection And Crohn’s Disease
What is the brain–gut axis?
Often called the second brain, your gut has a network of neurons more complex than the brain itself and is deeply involved in the process of dealing with emotions, almost like the brain deals with thoughts.
It’s a neural-neuroendocrine circuit connecting:
- The brain’s hunger–satiety centers.
- The hormonal reward system.
- The gut microbiota.
This axis regulates emotions, food choices, and digestive health.
Impact of modern diets:
- High sugar and high-fat diets disrupt this natural circuitry.
- These foods overstimulate the brain’s pleasure and reward system.
- Can result in patterns of addiction-like behavior. (13)
Mental health connection:
- The brain–gut axis links addiction, depression, and anxiety with digestive conditions.
Living with Crohn’s or bowel conditions may trigger feelings of:
- Worry or embarrassment.
- Sadness or depression.
- These emotions may create a psychosomatic (mind–body) influence, worsening gut symptoms.
Why mindset matters:
- The gut has been called our “emotional brain.”
- Negative attitudes and beliefs can aggravate intestinal conditions.
Positive thinking, emotional healing, and belief systems can:
- Improve gut function.
- Reduce symptom severity.
- Support long-term health outcomes.

Mind–Body Healing and Crohn’s Disease
Because up to 80% of the mind is subconscious and is structured around past events, unresolved trauma or grief, and also the voices of peers, parents and outside influences, techniques to explore and control our thoughts are crucial to our long-term health.
Harness the power of the mind:
- The mind is a powerful healing tool.
- Positive thinking can influence both mental health and physical healing.
- Cultivating optimism and hope supports immune balance and digestive recovery.
Healing practices to explore:
- Meditation – calms the nervous system, reduces stress, and strengthens the brain–gut axis.
- Reading uplifting material – nourishes the mind with positive thoughts.
- Social activity – engaging with a supportive circle of kind friends provides emotional resilience.
- Energy healing, massage, and relaxation techniques – encourage both emotional release and physical relaxation.
Practical approach:
- Find a practice that resonates with you personally.
- Make time for regular learning and practice.
- Integrate mind–body strategies alongside nutrition and herbal remedies for a comprehensive healing plan.
Next steps:
- Begin by exploring guided meditation practices or local community classes.
- Consider building a daily self-care ritual that includes relaxation, emotional support, and mindfulness.
READ MORE ABOUT MEDITATION HERE
I hope this has been helpful and has given you new hope in your search for solutions. Check out the Ultimate Crohn’s Program below. With a little time and effort, you can potentially say goodbye to Crohn’s.
Brett Elliott ®

The Ultimate CROHN'S DISEASE Program
The great thing with herbal medicines is that they have a long history of healing the digestive system and restoring gut health, in the area where modern and medicine really struggles.
When all else has failed herbs can come to the rescue. The secret is to getting a nice rounded combination of herbs and a good dosage while following the diet recommendations above, and also utilising the power of your mind. This is what I call the healing triangle.
Let’s look at the individual parts to the herbal program.
Aloe Vera - Healing The Gut Wall
Why Aloe Vera?
Considered one of the most powerful natural remedies for healing the gut wall over the long term.
Has a strong reputation for tissue repair, commonly used for burns, wounds, and internal healing.
Science and active compounds:
- Aloe vera gel contains over 200 active components.
Its exact healing mechanism is not fully understood, but it is known to:
- Promote tissue regeneration.
- Support gut lining repair.
- Reduce inflammation and irritation.
Forms and recommendations:
- Use pure aloe vera gel or juice with no additives or preservatives.
- You can also grow aloe vera at home and make fresh juice yourself.
Suggested dose:
- Take 30 mL daily, first thing in the morning, on an empty stomach.
Consistency is key for long-term gut wall healing.

L-Reuteri Probiotics - Improve Gut Microbiome
I suggest using the powerful Human prebiotic strain L-Reuteri, which you can get in the product called BioGaia. Take 2 tablets daily for the first month and 1 tablet daily for the second month.
Click here to find out more. DOSE: Take 1 tablet with water just before Dinner
BodiClenz - Herbal Intestinal Cleanse
One of the most effective things I have seen help with Chrohn’s Disease is the 14-day herbal Bodiclenz program. It contains a combination of 24 herbs designed to support bowel health and digestive processes. You simply take the powder twice a day and a smoothie for two weeks.
I highly recommend using these two recipes every day if possible, StomachClenz and BowelClenz.
DOSE: Take 2 scoops daily in a smoothie as your Breakfast and Lunch
ColonEze - Bowel Soothing Tonic
Some of the anti-inflammatory herbs traditionally used to encourage healthy microflora, heal the gut wall, and reduce negative bacteria and parasites include the following herbs, all of which are contained in the BodiClenz formulation.
– Licorice
DOSE: Take 10ml twice daily away from food. Repeating some of these herbs in a liquid formulation, and adding a couple of extra anti-inflammatory, immune-supporting herbs in a liquid will help increase the effect of the powered herbs taken in a smoothie.
See the ColonEze Liquid Formulation Here Herbal Teas to reduce inflammation and intestinal permeability:

ColonEze Herbal tea
– Raspberry
– Peppermint
– Chamomile
– Ginger
Try a mixture of these teas in your teapot and drink 2-3 cups daily. You can get this blend pre-made here. You will just need to add some fresh ginger. DOSE: Take 2-3 cups daily from a teapot, great in the evening.

The Ultimate Herbal ColonEze Program Complete
Get everything in one complete package, and save 30%. The Ultimate IBS and Crohn’s Program comes with everything you need for the full 1-month treatment program. Click Here to Find out more
Note: Intestinal permeability
The gut barrier plays a key role in the avoidance of inflammatory responses to the microflora and is regulated by a finely tuned network of immune mechanisms (3)
Because increased intestinal permeability and inflammation go hand in hand, natural methods to reduce intestinal inflammation will be useful. A diet rich in plant and vegetable fiber has been shown to greatly reduce inflammation.
A recent demonstration from the Nurses Health study that subjects had a 50% lower risk for the development of Crohn’s disease, which was directly associated with long-term ingestion of a diet rich in fruit and vegetable fiber. (13)
The Herbal Detox diet plan promotes a pure fruit and vegetable diet and has been reported to assist with inflammatory bowel disease. Powerful triggers for inflammation are the presence of microorganisms in sites where they do not belong. Microorganisms contain structures alien to the body.
Bacteria and fungi, for example, have cell walls in contrast to human cells that lack these structures, and viruses have unique forms of DNA and RNA. Cells and molecules involved in the inflammatory defense system react immediately against these foreign elements; they are danger signals to the body. (15)
Again this points to supporting the microflora, as above, which also introduces antiparasitic, antifungal, and anti-inflammatory agents. Traditional herbal remedies include:
More About Meditation
Going back to the brain-gut connection, there is an important role for the nervous system to play in Crohn’s Disease. Meditation can play a major role here. One randomized controlled trial demonstrated that mindfulness training has a substantial therapeutic effect on bowel symptom severity, improves health-related quality of life, and reduces distress. (7)
Interestingly, changes in quality of life, psychological distress, and visceral anxiety were not significantly different between groups immediately after treatment but evidenced significantly greater improvements in the meditation group at the 3-month follow-up.
(7) This makes sense, as the effects of meditation are known to increase over time. Read more Here